Fecal impaction testing and diagnosis
How getting the right tests can save your life
It is now well established that patient communication is the best diagnostic tool a doctor has to correctly identify a fecal impaction. However, research also shows that there is often a disconnect between doctors and patients when it comes to diagnosing constipation
This is why, you, the patient, are in the best position to guide your doctor in getting the proper tests and choosing he correct therapeutic approach to reverse your problem.
There are many benefits to getting accurately diagnosed early on…
- The slower your stool moves, the bigger it gets.
- You can effectively break the cycle of recurrent fecal impactions
- You can avoid treatments that might be wrong for your particular case
- You can prevent fecal impaction injuries to your kidneys and bladder
- You lower your risk of colon cancer from chronic gut inflammation
- You can reduce and even eliminate your risk of mortality from fecal impactions
- Most importantly, you can return your digestive tract and your overall health back to normal
Going to a doctor and getting properly tested isn’t just about just knowing whether you have a fecal impaction or not. You may already have that answer.
It’s about knowing other crucial details about your condition:
- What is the extent of your stool blockage?
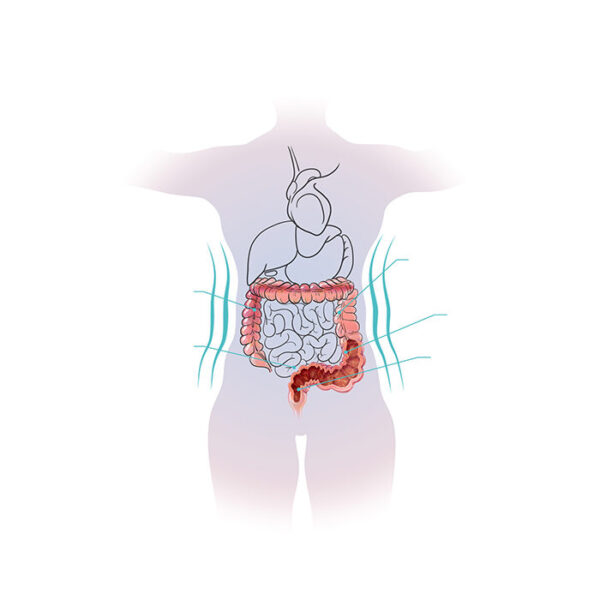
- What part of the intestine is your stool stuck in?
- Are there any signs of a gut infection?
- Is the inner lining of the colon affected?
- Has your colon wall weakened or thickened?
- Are your intestinal muscles functioning properly?
- Is there any bleeding or sign of a tear in your digestive tract?
- How much injury has your anorectal tissue experienced?
- Are nearby organs being damaged through something called the “mass effect”?
By insisting on getting tests that answer all these questions, you leave nothing to chance and neutralize fecal impaction’s silent but deadly threat. In other words, you ensure that you won’t be caught off-guard like so many other sufferers and become a scary statistic.
So, here are some tests you might want to consider discussing with your doctor…

A Comprehensive medical history
Every good checkup should start with asking you about the following things:
- Past and current medical problems (both physical and psychological conditions)
- Past surgeries, procedures or hospitalizations
- What medications you take (including natural supplements)
- Allergies or reactions
- History of smoking, alcohol or drug use
- Family history (what conditions run in your family)
Then there might be questions specific to your fecal impaction…
- How often you go to the bathroom?
- When was the last time you passed stool?
- Do you have constipation and how often do you experience it?
- Do you use any products for your constipation?
- How much water do you drink a day and what is your fiber intake like?
- How much activity do you get a day and is your work desk-bound or active?

A thorough physical exam
Your doctor should check your abdomen for distension, tenderness and palpable hard lumps.

A digital rectal exam
While some physicians are averse to this, be sure to choose a doctor that performs this test. It is an instant way to detect a hard mass in the rectum. A good doctor can even use this method to tell if your resting rectal pressures are reduced (which would indicate a problem with your anorectal muscles).

Anorectal manometry
This is an even more advanced test that checks whether your rectal and anal sphincter muscles are functioning properly.

X-Ray
If a fecal impaction is suspected, your doctor may order something called an acute abdominal series. This allows them to visualize your digestive tract using x-ray imaging. An x-ray can reveal any lodged fecal mass, bowel obstructions and even free air under the diaphragm (which would indicate a tear in the colon through which air has escaped into the peritoneal cavity).

Barium enema
This method still uses an x-ray, except your colon is filled with a liquid (barium sulfate) that shows up brightly during imaging. A barium enema gives a clearer picture of your colon, its size, its shape and even the state of its inner lining.

Fluoroscopy
Used in conjunction with a barium enema, fluoroscopy uses a continuous x-ray beam that shows real-time images of your colon. This allows the doctor to visualize the movements of the intestine and identify any functional disorders your colon might have.

CT Scans
This is one of the most detailed ways to visualize your colon. CAT scans are more sensitive than x-rays. They can show colon perforations, wall thickening and even ischemic damage that occurs when the blood flow within your gut is affected from an impacted stool.

Sitz marker exam
For this test, you’re asked to ingest a capsule that contains tiny plastic rings. These rings show up on x-rays as they make their way through your entire digestive system. By checking how long it takes you to clear all the rings, your doctor can assess if something is wrong with the nerves or muscles of your digestive tract.

Sigmoidoscopy
While imaging of the gut is a great way to examine it from the outside, there is no substitute for visually inspecting the digestive tract from the inside. This method uses a flexible camera to check your rectum and the last portion of your colon (sigmoid) because this is where most fecal impactions occur.

Colonoscopy
When a doctor wants to visualize your entire large intestine from the inside, they often recommend a colonoscopy. This allows the gastroenterologist to check for abnormalities in your colon tissue and look for signs of colon and rectal cancer.

Colon Biopsy
If your doctor does see anything concerning during a sigmoidoscopy or colonoscopy, they might take a tiny piece of the tissue so that it can be examined later in a lab. A microscopic analysis of the tissue can often identify abnormalities at a cellular level which can prevent major complications down the line.

Blood tests
As part of your complete checkup, your doctor should order you a complete blood count with differential (CBC) and a basic metabolic panel (BMP). The results from these tests should allow your doctor to identify things like internal bleeding and gut infections. It can even detect if your fecal impaction is affecting other organs such as your kidneys, liver, pancreas, etc.

Fecal occult blood test (FOBT)
This test checks for hidden blood in your stool which can indicate a tear in you digestive lining, colitis, polyps or even colon cancer.
While this list isn’t meant to be exhaustive, it should give you a good idea of what tools your doctor has to evaluate your actual condition regardless of what your symptoms are suggesting.
Here are a few more tips to help you ensure that your diagnosis is accurate…
- Get a checkup as soon as you can, especially if it’s been more than 6 months
- If possible, see a gastroenterologist instead of general practitioner
- If you are exhibiting any of the 15 emergency signs of fecal impactions, go to the ER immediately
- Go in prepared with your detailed medical history and a list of questions to ask your doctor
- You ideally want a doctor that is meticulous as a clinician and addresses all your concerns
- Make sure your doctor is attentive and not averse to a rectal exam
- Bring up the tests mentioned above even if your doctor doesn’t – sometimes all it takes is a suggestion to catch a looming threat
- Be open with your doctor and don’t be embarrassed to discuss your problem
- If an enema is recommended, ask if you can get one in a clinical setting
- Go back to the doctor if you still haven’t passed stool or if a new symptom arises
* If a doctor or a nurse is about to give you an enema, make sure you tell them if you have hemorrhoids, fissures or digestive issues such as ulcerative colitis because this can increase your chances of serious complications.
By getting accurately diagnosed, you lift the veil behind which fecal impaction carries out its hidden damage. You finally become aware of your colon’s true health and are able to take charge of its healing.
What’s surprising though is that the hardest thing about successfully treating a fecal impaction isn’t just identifying what is really happening inside you and choosing the right therapeutic approach, it’s overcoming the sheer amount of misinformation that is often found on the internet. For example, one of the most common pieces of advice given to constipation and fecal impaction sufferers is to try a laxative or an enema. We now know that this advice is harmful to the sufferer because these products actually worsen your functional bowel disorder in the long run.
There are many other commonly believed myths that trick you into trying ineffective treatments that don’t prevent your bowel disorder from progressing further or worse, these myths also deceive you into a false sense of calm even when your digestive tract is under an advanced state of breakdown.
If you want to avoid falling into the same traps as others and want to ensure that your digestive tract permanently returns to a healthy state, it is important that you become aware of the 15 most dangerous myths about constipation and fecal impaction.



